When living with metastatic colorectal cancer (mCRC)...
CYRAMZA can help keep you fighting for what matters to you
CYRAMZA, in combination with FOLFIRI (irinotecan, folinic acid, and fluorouracil), is indicated for the treatment of patients with metastatic colorectal cancer (mCRC) with disease progression on or after prior therapy with bevacizumab, oxaliplatin, and a fluoropyrimidine.
SELECT SAFETY INFORMATION
CYRAMZA may cause serious side effects, including:
Tears in the stomach or bowel wall may happen with CYRAMZA. This can be life threatening. Tell your doctor if you have severe diarrhea, vomiting, or severe abdominal pain. If you have tears in the stomach or bowel wall, you will have to stop receiving CYRAMZA.
You're not the type to settle. You're the type who pushes for more. But where individual results with CYRAMZA can vary, clinical studies have shown...
CYRAMZA may help you live longer
56% of people lived 1 year or longer with CYRAMZA + FOLFIRI (a type of chemotherapy) vs 48% with chemotherapy alone
- Half of the people who received CYRAMZA + chemotherapy after their cancer progressed were still alive at 13.3 months vs 11.7 months with chemotherapy alone

CYRAMZA provided more time without disease progression
47% of people had delayed disease progression for 6 months or longer with CYRAMZA + chemotherapy vs 36% with chemotherapy alone
- Half of the people who received CYRAMZA + chemotherapy lived without their cancer getting worse for 5.7 months vs 4.5 months with chemotherapy alone
CYRAMZA was studied in a clinical trial of 1072 people with metastatic colorectal cancer who received CYRAMZA + FOLFIRI (536 people) vs those who received FOLFIRI alone (536 people). All people in the study had previously received bevacizumab, oxaliplatin, and a fluoropyrimidine (other types of chemotherapy).
SELECT SAFETY INFORMATION
CYRAMZA may cause serious side effects, including:
Wounds may not heal quickly or completely. Tell your doctor if you have a wound that doesn’t heal properly or have a surgery planned. If you are having surgery, CYRAMZA treatment should be stopped beforehand. Your doctor may put you back on CYRAMZA after your surgical wound has healed.
Explore the Lilly Oncology Support Center for information on savings and financial assistance.
What to expect during treatment
You’ve decided to move forward and are ready to start treatment. Let’s do this.
Treatment will be given by an intravenous (IV) infusion, in either the doctor's office, a hospital, or an infusion center.

CYRAMZA is given in combination with FOLFIRI. Both CYRAMZA and FOLFIRI are given by intravenous infusion [Fluids or medication given into a vein by means of a needle or catheter], commonly referred to as an IV. The medicines will be delivered into your vein. A doctor or nurse will give you treatment at the doctor’s office, a hospital, or an infusion center.
Before you receive treatment with CYRAMZA, your doctor will administer different medications to help prevent an allergic reaction that may occur during infusion.
When you receive CYRAMZA with FOLFIRI, treatment will be given on the first day of a 14-day cycle. Your doctor will determine the number of treatments you receive. CYRAMZA and FOLFIRI will be given once every 2 weeks, or as recommended by your doctor. The first CYRAMZA infusion will take about 60 minutes, followed by FOLFIRI. If you handle the first infusion of CYRAMZA well, then your next CYRAMZA infusions may take only 30 minutes.

CYRAMZA combines with FOLFIRI (a type of chemotherapy) to help fight your cancer.
Understanding your dosing schedule with CYRAMZA
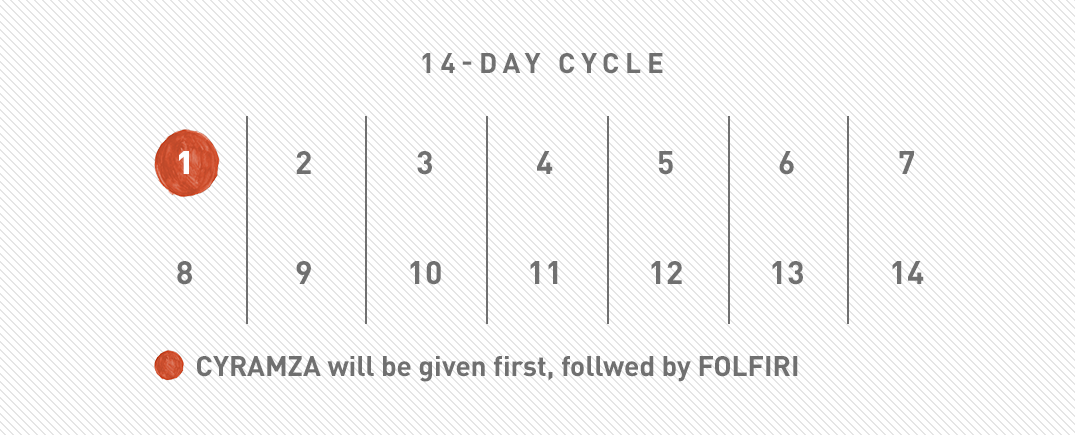
CYRAMZA + FOLFIRI (A TYPE OF CHEMOTHERAPY)
CYRAMZA + FOLFIRI will be given to you once every 2 weeks, or as recommended by your doctor.
Your doctor will determine the number of treatments you receive.
SELECT SAFETY INFORMATION
CYRAMZA may cause serious side effects, including:
Reactions related to infusing CYRAMZA have happened. These can be severe and life threatening. Most of these reactions happened during or after the first or second CYRAMZA infusion. Symptoms of infusion reactions include shaking or stiffness of the body, back pain or spasms, chest pain or tightness, chills, flushing (sudden warmth and/or reddened skin on the face, neck, or upper chest), difficulty breathing, wheezing (a whistling sound in the breath caused by narrowed breathing tubes), becoming blue due to lack of oxygen, and tingling or numbness of the skin. In severe reactions, rapid heartbeat, low blood pressure, and severe trouble breathing may happen. Your healthcare team will give you medicine before each CYRAMZA infusion and will watch you for these side effects. If a reaction happens,CYRAMZA treatment may be infused at a slower rate or may be permanently stopped, depending on how severe the reaction is.
Tips for day of treatment and beyond
You may be nervous about your first treatment. Or maybe you're an old pro at this. But no matter where you're coming from, here are some important tips to help get you through each infusion with CYRAMZA:
Eating healthy and living well
When living with colorectal cancer, good nutrition is essential. Talk to your doctor about strategies that can help keep you eating healthy. He or she might recommend eating multiple small meals a day to help you maintain weight and balance your blood sugar. Your doctor might also mention incorporating more high-protein foods, like:
Fish
Lean meats
Cooked Vegetables

Smoothies
However, maintaining a nutritious diet can be difficult if you’re too tired to eat or having trouble keeping anything down. You may be experiencing side effects from treatment, like nausea or mouth sores, that also may cause you to lose your appetite.
You may be feeling frustrated. It can be hard to retrain your body to eat in this new way. And if you’ve had a colostomy, there may be some foods that you might need to limit—and some that might be helpful—in order to better manage your colostomy bag. Food you might need to limit include raw vegetables, fruit skins and peels, dairy products, high-fiber food, beans, peas, lentils, brown and wild rice, nuts and seeds, sweets, and high-fat and fried foods. Foods that can be helpful include cranberry juice, bananas, apple sauce, well-cooked sticky white rice, buttermilk, tapioca, and white toast. It’s important to listen to your body and communicate any changes in bowel habits (including diarrhea, constipation, bloating, and gas) to your healthcare team.
In addition to eating right, it’s important to keep balance in your life. Reducing stress can help you feel energized, so you can focus on the things that matter most. Stress-reducing activities include:
Exercise
Resting
Yoga or meditation
Understanding common side effects
CYRAMZA in combination with FOLFIRI (a type of chemotherapy) may cause side effects. If you experience new symptoms while on treatment, it is important that you speak with your doctor.
Explore the most common side effects of CYRAMZA, below.
The most common side effects were:
Diarrhea; low white blood cell count; decreased appetite; nosebleeds; mouth sores; low platelet count; high blood pressure; swelling in the arms, legs, hands, and or feet; too much protein in the urine; hand-foot syndrome; bleeding in the gastrointestinal tract; low albumin (a protein in the blood)
The most common serious side effects were:
Diarrhea, blockage of the intestine, and low white blood cell count with fever
Talk to your doctor about any questions, concerns, or side effects you might have with CYRAMZA. Your doctor may be able to make recommendations to help you feel more comfortable.
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/safety/medwatch or call 1-800-FDA-1088.
Please see Safety Summary for more safety information for CYRAMZA.
